The common belief is that with assisted reproductive technique, there is a high probability of having twin or multiple pregnancies. Many couples who visit a fertility clinic share their concerns regarding having twins or multiple pregnancies with the IVF procedure. However, the risk of multiple pregnancies is only in the case of certain IVF procedures and not all.
In general, the possibility of IVF twins percentage is 3% and is triplets 0.1%. The statistics for IVF twins is 25%, and the likelihood of triplets is 4%. It has, however, been noticed that over recent years, multiple pregnancies are becoming more common with natural pregnancies. This could be due to the fact that women now have children when they are older. Age increases the likelihood of multiple pregnancies.
Women who undergo IVF treatment can expect to have multiple pregnancies due to a number of different factors related to the procedure. Under the IUI treatment where the sperm of the male partner is injected into the woman uterus, there is a high possibility that more than one egg may fertilise leading to multiple pregnancies. In this procedure, the sperm is washed, and only the healthy ones are injected into the female partners’ uterus. Since the sperm used, are mainly of good quality, and they are in the vicinity of the eggs, there is a possibility that multiple eggs may get fertilised. This is not a rule, and generally, IUI results in a single pregnancy.
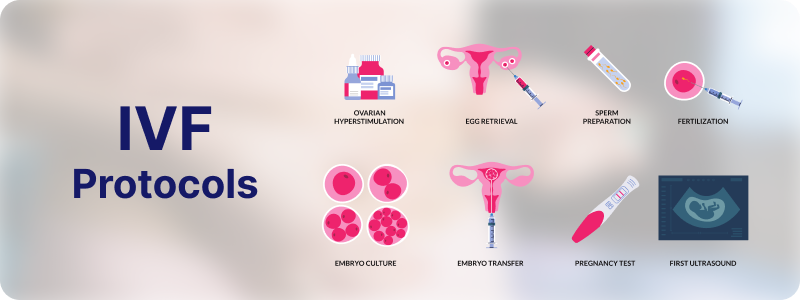
In vitro fertilization (IVF) is a complex procedure that involves fertilizing an egg with sperm outside of the body, typically in a laboratory setting. IVF protocols encompass a series of steps designed to optimize the chances of successful fertilization, implantation, and ultimately pregnancy. These protocols can vary depending on individual patient characteristics, reproductive history, and clinic preferences. In this 1500-word overview, we'll delve into the key components of IVF protocols, including patient evaluation, ovarian stimulation, egg retrieval, fertilization, embryo transfer, and post-transfer care.
The IVF journey begins with a thorough evaluation of both partners to assess their fertility status. This evaluation often includes a comprehensive medical history review, physical examination, and various diagnostic tests. For women, these tests may involve assessing ovarian reserve through blood tests for hormone levels (e.g., FSH, AMH) and antral follicle count via ultrasound. Men may undergo semen analysis to evaluate sperm count, motility, and morphology. Additionally, both partners may undergo infectious disease screening and genetic testing to identify any potential risks or concerns.
Once the evaluation is complete, ovarian stimulation is typically initiated to increase the number of eggs available for retrieval. This involves the administration of fertility medications, commonly gonadotropins such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH), either alone or in combination with other medications like gonadotropin-releasing hormone (GnRH) agonists or antagonists. These medications help to promote the growth and maturation of multiple follicles within the ovaries, each containing an egg. The stimulation protocol may be adjusted based on the patient's age, ovarian reserve, and previous response to treatment.
Throughout the ovarian stimulation phase, patients undergo regular monitoring through blood tests and transvaginal ultrasound to track follicular development and hormone levels. This monitoring helps to determine the optimal timing for triggering final egg maturation and ovulation. Human chorionic gonadotropin (hCG) or a GnRH agonist may be used as the trigger medication, administered when the follicles have reached an appropriate size and the endometrium is adequately prepared.
Approximately 36 hours after trigger administration, the egg retrieval procedure is performed. This is typically done under sedation or anaesthesia to ensure patient comfort. Using transvaginal ultrasound guidance, a thin needle is inserted through the vaginal wall and into each ovarian follicle to aspirate the fluid and contents, including the eggs. The retrieved eggs are then immediately transferred to the laboratory for fertilization.
In the laboratory, the retrieved eggs are combined with sperm for fertilization. Depending on the specific circumstances of the couple, fertilization may occur through conventional insemination, where sperm are placed in close proximity to the eggs in a culture dish, or through intracytoplasmic sperm injection (ICSI), where a single sperm is directly injected into each mature egg. Following fertilization, the resulting embryos are cultured in a controlled environment for several days, typically up to five or six days.
As the embryos develop, they are closely monitored for signs of quality and viability. This may involve assessing factors such as cell number, size, symmetry, and the presence of fragmentation. In some cases, additional techniques such as preimplantation genetic testing (PGT) may be used to screen embryos for chromosomal abnormalities or genetic disorders. Based on these evaluations, one or more embryos of the highest quality are selected for transfer.
The embryo transfer procedure typically occurs three to five days after egg retrieval, although in certain cases, embryo transfer may be delayed until the blastocyst stage (around day five or six). Prior to transfer, the chosen embryos are loaded into a thin, flexible catheter, which is then carefully guided through the cervix and into the uterus under ultrasound guidance. Once in the desired location, the embryos are gently released into the uterine cavity, where they may implant and develop into a pregnancy.
Following embryo transfer, luteal phase support is often provided to help facilitate implantation and support early pregnancy. This may involve the administration of progesterone supplements, either vaginally, orally, or via injection, to mimic the natural hormonal environment of the luteal phase. Luteal phase support typically continues for several weeks until pregnancy can be confirmed through blood tests measuring levels of human chorionic gonadotropin (hCG).
Approximately two weeks after embryo transfer, patients undergo a blood test to measure hCG levels, which can indicate whether implantation has occurred and pregnancy has been established. If the test is positive, further monitoring may be scheduled to assess the progression of the pregnancy through ultrasound imaging and additional blood tests. Depending on the outcome, ongoing prenatal care may be provided, or alternative options may be discussed if the IVF cycle was unsuccessful.
In summary, IVF protocols encompass a series of coordinated steps aimed at optimizing the chances of successful fertilization, implantation, and pregnancy for individuals struggling with infertility. Through a combination of ovarian stimulation, egg retrieval, fertilization techniques, embryo evaluation, and supportive care, IVF offers hope to couples seeking to build their families. While each patient's journey is unique, the overarching goal of IVF protocols remains the same: to achieve the dream of parenthood.